2021 is rapidly approaching and eMedApps wants healthcare organizations to be aware of the 2021 MIPS (Merit-based Incentive Payment System) Final Rules. Below we have a few categories with updates that should be reviewed to ensure that reporting goes smoothly in the upcoming year.
Traditional MIPS Performance threshold and category weights
- The performance threshold is set at 60 points to avoid a MIPS penalty.
- The additional performance threshold for exceptional performance will remain the same at 85 points.
- There are no changes to the MIPS payment adjustments which will stay at +/- 9%. MIPS eligible clinicians who do not report MIPS in 2021 will receive a -9% MIPS penalty against their 2023 Medicare Part B payments for covered professional services.
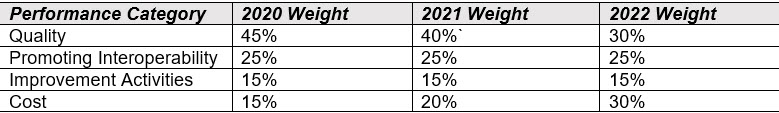
By law, the Cost and Quality performance categories generally must be equally weighted at 30% beginning in the 2022 performance period.
Performance Categories: Traditional MIPS
Quality performance category:
- Changes to 113 existing MIPS quality measures (7 of which had substantive changes that don’t allow comparison with historical data).
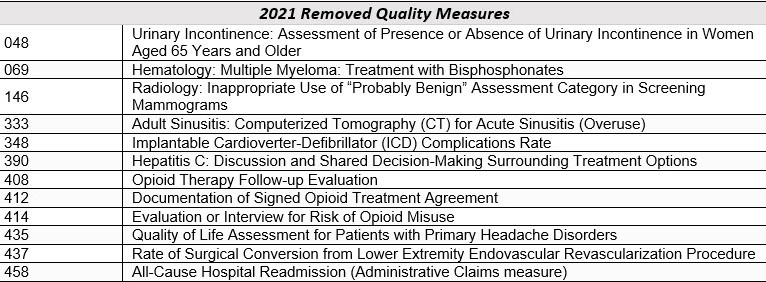
- Removed 11 quality measures from the MIPS program as well as the All-Cause Hospital Readmission measure
- 2 new administrative claims measures added, including the Hospital Wide Readmission measure.
- Revised scoring flexibility for measures with specification or coding changes during the performance year; and
- Sunset the CMS Web Interface as a collection and submission type but will extend the availability of the CMS Web Interface as a collection and submission type for one year for the 2021 performance period.
Cost performance category:
- Update existing measure specifications to include telehealth services that are directly applicable to existing episode-based cost measures and the Total Per Capita Cost (TPCC) measure.
- Weight the Cost performance category at 20% for individuals, groups, and virtual groups reporting traditional MIPS.
- Weight the Cost performance category at 0% for APM Entities reporting traditional MIPS.
Improvement Activities performance category:
- CMS has removed IA_CC_5 CMS Partner in Patients Hospital Engagement Network
- Modified 2 activities for 2021:
- IA_BE_4 Engagement of patient through implementation of improvements in patient portal
- IA_AHE_7 Comprehensive Eye Exams
- Continue the COVID-19 clinical data reporting Improvement Activity with a modification to the activity description.
Promoting Interoperability performance category:
- Retained the Query of Prescription Drug Monitoring Program (PDMP) measure as an optional measure and finalized to make it worth 10 bonus points.
- Changed the name of the Support Electronic Referral Loops by Receiving and Incorporating Health Information by replacing “incorporating” with “reconciling.”
- Added an optional Health Information Exchange (HIE) bi-directional exchange measure as an alternative reporting option to the 2 existing measures for the HIE objective.
- Update certified electronic health record technology (CEHRT) requirements in response to the ONC 21st Century Cures Act Final Rule.
Have any questions or need clarification on any of the new rules? We are here to assist, feel free to contact us here.

